God Willing, He Will Cure Cancer, and Shrimp
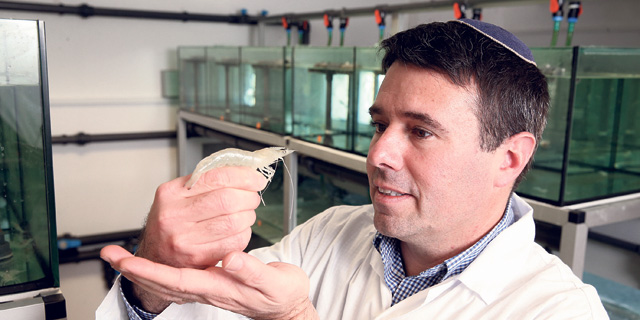
At 43, Technion researcher Avi Schroeder is a phenomenon with four startups under his belt, working to cure cancer with elephant protein and trying to personalize chemotherapy. In between, the kosher-keeping Yeshiva graduate is taking on a deadly shrimp plague
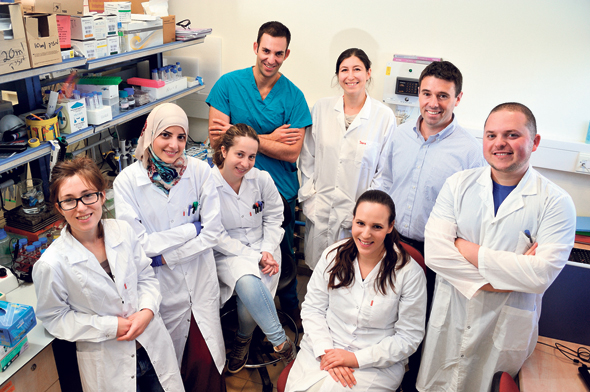
Avi Schroeder’s lab at the Technion Israel Institute of Technology is tiny but mighty. Thirty researchers crowd it daily, covering areas such as biology, chemistry, medicine, pharmaceuticals, and even mechanical engineering. The lab is part of the chemical engineering faculty, but the researchers here were handpicked from different departments to serve the lab’s interdisciplinary mission. The content of the multitude of test tubes here could one day result in life-saving medication for a variety of conditions. Until then, the lab has already birthed several innovations that matured into business ventures: Schroeder and his team are involved in four such companies based on the lab’s scientific breakthroughs, ranging from using elephant protein to cure cancer to personalizing chemotherapy.
At 43, Schroeder is a research phenomenon. He completed his chemical engineering PhD at the age of 33, continued to a post-doctorate at the Massachusetts Institute of Technology, and by the age of 36 was one of Israel’s youngest professors. Seven years ago, he set up one of the country’s leading nano-medicine labs. His primary tools are liposomes, vesicles that can be used as a drug delivery system thanks to their ability to encapsulate hydrophilic or lipophilic drugs. His life’s work is to advance liposome-based cancer treatments. While there’s still work to do on that front, Schroeder’s innovations to date have brought on a surprising twist for the kosher-keeping, yarmulke-wearing yeshiva graduate: for the past few years, he has been busy curing that very unkosher crustacean, the shrimp. To his mother, Schroeder initially said he was working on a cure for cancer, which was a white lie—in Hebrew, the same word is used for both cancer and crab. He considers himself a liberal person, one who doesn’t care about what other people put on their plates, he said. “The important thing for me is that I am saving a crucial food source for many people. Indeed, people here sometimes tease me about the fact that I don’t know how tasty shrimp is and about what I’m losing out on, but I don’t care about that.” The connection between Schroeder and shrimp was accidental, the result of his specialization in drug delivery methods. Six years ago, he gave a lecture at Israeli pharmaceutical company Protalix BioTherapeutics, where he met molecular biologist Shai Ufaz, then a Protalix employee and today a business partner and the CEO of their joint company ViAqua Therapeutics Ltd. Ufaz found the lecture enlightening. He previously worked for a marine agriculture company and understood the span of the damage shrimp growers contend with. Hearing the lecture, it dawned on him that Schroeder’s direction could offer a solution to a very wide-spread problem. The disease Ufaz was thinking about is white spot syndrome, a virus that affects a wide variety of crustaceans and is viral among shrimp, especially in east Asia, where most commercial farming—an industry with an annual turnover of over $30 billion—is located. An infected shrimp farming pond has a mortality rate of around 80%, with deaths occurring within hours of infection. To date, most attempts to control the virus and prevent it from spreading to other parts of the world focused on bettering sanitation and thinning out the animals, but these measures are only partly effective. The syndrome causes damages of around $6 billion a year, according to ViAqua’s data. A week after the Protalix lecture, the scientists met. Ufaz and another eventual ViAqua co-founder, marine biologist Shai Einbinder, told Schroeder about the problem. There was a bit of squirming and skirting around the issue before they dared say the product they wanted to develop was for shrimp, Schroeder recalled. In 2014, they banded together to form the company. In a little cabin at the edge of the Technion’s campus, a few dozen small aquariums have a great view of Haifa bay. Inside those containers, thousands of ViAqua’s test shrimps await their midday meal. There is one special ingredient inside the little food pellets they receive—a food additive that should provide immunity to the virus. “We created a substance that is made of a shrimp’s usual food sources, so it is defined as a food additive and not a drug,” Ufaz explained. “We want to reach the shrimp when they’re still young and inoculate them against the disease before they have a chance to catch it.” The Technion cabin only hosts ViAqua’s base trial, for the pellet formula. As Israel forbids bringing the white spot syndrome virus into the country, even for research purposes, the company’s clinical trial is held in three locations in Europe, Asia, and the U.S. Company data shows inoculated shrimp experience a drop of over 50% in mortality rates. ViAqua’s vaccine is based on RNAi. In 1998, American researchers Andrew Fire and Craig Mello discovered that RNA molecules can under certain circumstances, inhibit gene expression or translation. They won the 2006 Nobel Prize in medicine for their discovery, called RNA interference, or RNAi. “In 2012, when I arrived at MIT for my post-doc, the discovery of the RNAi mechanism was still completely new, and many people attempted to harness it for cancer-related applications, like the prevention of metastatic cancer,” Schroeder said. When cancer cells leave the original tumor and invade the lungs, for example, they require a certain protein to attach themselves to lung tissue. It has been proven that if the production of that protein is delayed, there is less metastation, Schroeder said. “We can synthesize a molecule called siRNA, which knows to replace the body’s original RNA. We can create this molecule with a certain sequence that will stop cells from becoming infected and metastating, and such a molecule with a different sequence will make the cell more vulnerable to drugs.” The process is the same in both humans and shrimp, Schroeder explained. “For the virus to pass from one cell to another in shrimps, it needs certain proteins, the production of which we now know how to stop.” In shrimps, though, there is only one protein responsible for the virus that needs targeting, while in cancer cells, there are multiple ones. ViAqua’s product is currently in the process of receiving regulatory approval in 11 countries, and if all goes well, it will hit the market within the next 12 months. The company, which forecasts revenues of 5 million euros for the first year, has recently signed an exclusivity agreement with Nutreco, one of the industry’s leading companies for animal nutrition and aquafeed. Nutreco NV also became a partner in ViAqua. Other company partners include the Technion, Israeli venture firm and accelerator Trendlines Group Ltd., and Singapore-based venture capital fund VisVires. Before shrimps, however, there was cancer. Schroeder’s first run-in with the disease was during his BSc days, when he studied chemical engineering at Ben-Gurion University of the Negev. At the time, he was a low-level employee at Teva Pharmaceutical Industries Ltd. who dreamt of a career as a pharmaceutical engineer. He was sent to assist at the lab of Hebrew University biochemist Yechezkel Barenholz, a medical nanotechnology pioneer and one of the developers of breast cancer treatment Doxil, the first liposomal drug and nano-medicine approved by the U.S. Food and Drug Administration. Barenholz was working to develop liposome-based technology for the safe conduction of chemotherapy drugs in hopes of finding a way to bypass chemotherapy’s debilitating side effects. While the project failed to reach commercialization, it changed Schroeder’s life. “I had no intention of continuing in academia, I wanted to develop drugs, but when I understood the things research can accomplish I realized my place was in academic research and not the industry,” he said. Schroeder’s first study with liposomes involved childhood cancer patients. No one likes getting jabbed with a needle, but children receiving chemotherapy experience that all the time, making their situation even harder, he said. Parents receive a topical numbing agent to spread on the child’s skin before leaving for the hospital, but traffic jams and patient backlog sometimes mean the numbing effect has passed by the time the staff gets to the child. To surpass that problem, Schroeder and his team worked to develop an ultrasound wave-based system that will lead the numbing agent directly to the needed location quickly. While they did manage to develop the system, they had no takers. The project did not fail so much as it was ahead of its time, Schroeder explained, adding that his paper on the research was cited over a thousand times. “It takes time for the scientific world to catch up to the technological and business world. When we approached the drug companies at the time and proved that the product works, they said ‘that’s nice, but we don’t deal with ultrasound,’ and ultrasound companies said ‘that’s nice, but we don’t sell drugs.’ Today, many of the new drugs integrate a technological system.” The next phase of Schroeder’s career was, again, accidental. In 2006, as a doctoral student at the Hebrew University of Jerusalem, the lab was approached by Hadassah University Hospital Ein Kerem regarding a child with a locked jaw. The hospital wanted to see if liposomes could be used to treat her. “We took empty liposomes, played with their molecular structure, and managed to turn them into lube, like grease in a machine’s bearings.” That development resulted in Moebius Medical, a joint venture between the Hebrew University, the Technion, and Hadassah, which leveraged the formulation to treat rheumatoid arthritis. In 2016, Moebius sold the licensing rights for the product to Mumbai-headquartered Sun Pharmaceutical Industries Ltd. In 2015, another little girl led to another of Schroeder’s ventures. He was approached by Rambam Hospital in Haifa regarding a baby with a rare brain tumor that the doctors were uncertain how to treat. “We collaborated with them to create a testing system reminiscent of an allergy test,” he explained. “When you test allergens, you inject a very small dose of allergen material and wait to see whether the skin reacts. Following the same principle, we took liposomes and filled each one with a minuscule dose of different chemotherapy drugs, 0.001 of the treatment dose, which we then injected the child with. That amount cannot cause harm, but was enough to understand which drug created the required reaction.” That innovative approach led to the baby’s complete recovery, and to the establishment of Barcode Diagnostics Ltd., which develops the method for wider application. At least a third of cancer patients receive an unsuitable drug, and it is very hard to predict how a drug will react once injected, Schroeder said. “Our technology enables better treatment compatibility for every patient. Currently, we’re developing a tool that enables doctors to receive a clear indication of whether a drug works or not within 48 hours at most. After a few years of animal trials, we’ll start a clinical trial with breast cancer patients in 2020.” Some may choose to rest on their laurels, but not Schroeder. He founded another company in 2015, PEEL Therapeutics, a collaboration between the Technion and the University of Utah to test the anti-cancer properties of a protein taken from elephants. For those who missed the pun, “peel” means elephant in Hebrew. Elephants do not get cancer, Schroeder explained. ”When you look at their cells and compare them to ours, you see one difference related to a gene called P53, which is known to inhibit the development of cancer cells. As we age, that mechanism ages as well, which is why cancer becomes more common the older you get. Humans have to make do with two copies of this gene, one from each parent, but elephants have 40 copies, and with such a high number cancer simply cannot develop. The way the gene is built also makes the mechanism more durable. What we aim to do is take P53 from elephants and, using a liposome-based delivery system, lead that elephant gene directly into the tumor we want to kill.” PEEL now creates that protein artificially in a lab, but the first copy was taken from a blood sample of an elephant in a U.S. zoo. The company is currently in a preclinical stage, having achieved proof of principle in 15 cancer types, including aggressive cancers such as brain and pancreas, Schroeder said, adding that the company expects to achieve a marketable drug within a few years.